Medicine Cabinet Minefield: How old prescriptions drugs are fueling an opioid addiction crisis
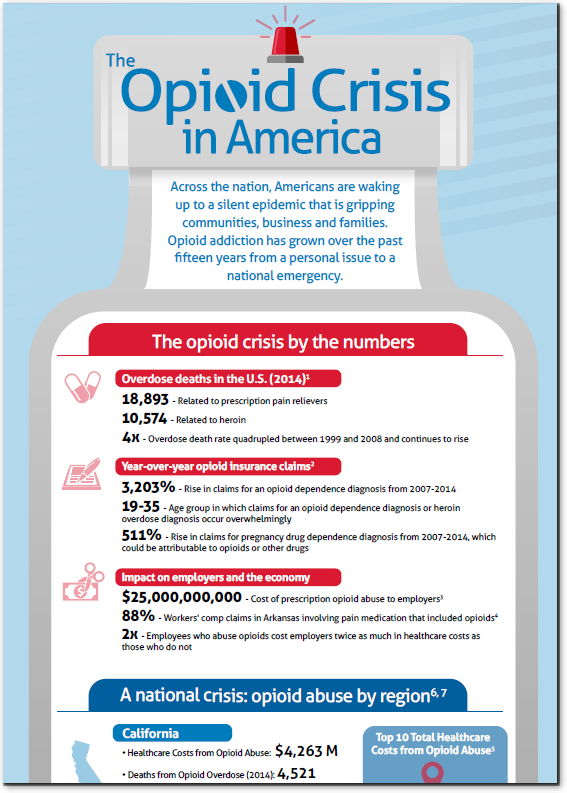
Opioid addiction kills thousands of people every year. In 2014, for example:
- There were 18,893 overdose deaths related to prescription painkillers
- There were 10,574 overdose deaths related to heroin
Despite these shocking numbers, the problem continues to grow. (It quadrupled in the first decade of this century and continues to explode). In the past twelve months, the Drug Enforcement Administration (DEA) has been forced to issue new warnings on drugs such as fentanyl, a potent opioid more than 100 times more powerful than morphine and 30-50 times stronger than heroin. While fentanyl has killed thousands of people over the past few years, many only heard of it recently, when it was attributed to the death of the musician Prince.
Close to Home: Opioid Addiction from Prescription Sources
Given the dangerous nature of some of the most common prescription painkillers—not just from concerns about addiction but from accidental and intentional overdose (the leading cause of accidental death)—it may be surprising to find out just how common it is to find opioid medications in the home.
In 2012, the Centers for Disease Control (CDC) calculated that healthcare providers wrote 259 million prescriptions for opioid painkillers. That is enough for every American adult to receive a bottle of pills.
While there have been efforts to reduce the number of prescriptions written, the number of prescriptions remains very high and the volume of opioid medications already distributed is also alarming.
And this is a key contributor to the opioid addiction crisis. According to the CDC, most people who abuse prescription opioids get them for free from a friend or relative. Essentially, people give their old prescribed medications to friends or relatives. Or, alternatively, abusers take old prescription pills from friends and relatives without their knowledge.
Even among the people at the highest risk of overdose (using prescription opioids non-medically 200 or more days a year) a friend or relative’s medicine cabinet is a common source of finding opioid medications. Among that population:
- 27 percent use their own prescriptions;
- 26 percent get them for free from family or friends;
- 23 percent buy them from friends or relatives; and
- 15 percent buy them from drug dealers.
Cleaning Up: Reducing the Availability of Prescription Opioids
Since the early years of the decade, state and federal authorities have made a concerted effort to reduce the regularity by which opioid medications are being prescribed. In particular, there has been a focus on reducing the ability of abusers to use multiple prescribers to issue painkillers.
Several states have achieved various degrees of success. In New York, the number of patients seeing multiple prescribers for painkillers was reduced 75% percent between 2012 and 2013 after prescribers were required to check the state’s prescription drug monitoring program before issuing a prescription.
In the same time-frame, Tennessee saw a 36 percent reduction in the number of patients seeing multiple prescribers for painkillers when it instituted a program similar to New York’s.
Florida saw a 50 percent reduction in oxycodone overdose deaths between 2010 and 2012 after it regulated painkillers and stopped providers from issuing painkillers from their offices.
In addition to programs aimed at healthcare providers, the Federal government has directed resources towards educating consumers about disposing prescription opioids and other medications. The Food and Drug Administration provides information on the safe disposal of painkillers such as Fentanyl patches. The Drug Enforcement Administration is also providing information for the public regarding disposal as well as created a program to authorize and register drug disposal collectors.
A Pioneer in Substance Use Management
Magellan Health is a pioneer in offering integrated, comprehensive opioid risk and substance use management programs. We have an unyielding commitment to ending the current epidemic. And we are uniquely positioned to bring together behavioral, medical and pharmaceutical programs to positively impact overall population health and reduce cost.